From CDC.
Invasive Methicillin-Resistant Staphylococcus aureus Infections Among Persons Who Inject Drugs — Six Sites, 2005–2016
June 8, 2018 / 67(22);625-628
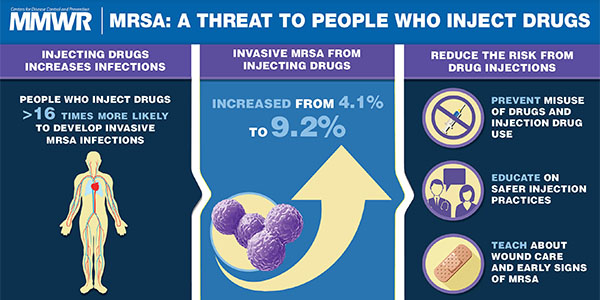
In the United States, age-adjusted opioid overdose death rates increased by >200% during 1999–2015, and heroin overdose death rates increased nearly 300% during 2011–2015 (1). During 2011–2013, the rate of heroin use within the past year among U.S. residents aged ≥12 years increased 62.5% overall and 114.3% among non-Hispanic whites, compared with 2002–2004 (2). Increases in human immunodeficiency virus (HIV) and hepatitis C virus (HCV) infections related to increases in injection drug use have been recently highlighted (3,4); likewise, invasive bacterial infections, including endocarditis, osteomyelitis, and skin and soft tissue infections, have increased in areas where the opioid epidemic is expanding (5–7). To assess the effects of the opioid epidemic on invasive methicillin-resistant Staphylococcus aureus (MRSA) infections during 2005–2016, surveillance data from CDC’s Emerging Infections Program (EIP) were analyzed (8). Persons who inject drugs were estimated to be 16.3 times more likely to develop invasive MRSA infections than others. The proportion of invasive MRSA cases that occurred among persons who inject drugs increased from 4.1% in 2011 to 9.2% in 2016. Infection types were frequently those associated with nonsterile injection drug use. Continued increases in nonsterile injection drug use are likely to result in increases in invasive MRSA infections, underscoring the importance of public health measures to curb the opioid epidemic.
Continue reading original article.
